Spinal cord stimulation (SCS) is a method designed to alleviate chronic pain associated with various medical conditions.
Developed in the late 1970s, SCS or spinal cord stimulators fall into the realm of neuromodulation techniques, This field also includes peripheral nerve stimulation.
Neuromodulation involves altering pain signal transmission within the spinal cord through the application of low electric currents via tiny electrodes.
Studies suggest that while spinal cord stimulators may not be universally effective, they typically reduce pain by approximately 50%, with roughly 65% of patients experiencing diminished pain following the implantation of a spinal cord stimulator.
Dr Meena Mittal at the Persistent Pain Solutions provides spinal cord stimulators for patients suffering from chronic neuropathic pain stemming from various underlying causes, including angina, complex regional pain syndrome, persistent post spinal surgery syndrome, pain from radiculopathy and neuropathic pain.
Spinal cord stimulation is often recommended where other treatments have not worked; note that a spinal cord stimulator may not completely eliminate pain but rather reduce it, decreasing reliance on pain medication.
Table of Contents
- What is a Spinal Cord Stimulator?
- How Does Spinal Cord Stimulation Alleviate Chronic Pain?
- Why Would You Get a Spinal Cord Stimulator for Chronic Pain?
- The Risks of Getting a Spinal Cord Stimulator
- Additional Issues to Consider With a Spinal Cord Stimulator Implant
- The Process of Getting a Spinal Cord Stimulator Implanted
- Preparing for a Spinal Cord Stimulator
- After Getting a Spinal Cord Stimulator Permanent Implant (Follow-Up)
- Getting a Spinal Cord Stimulator Removed
- Finding a Doctor Who Performs Spinal Cord Stimulation Near You
- Spinal Cord Stimulation at Persistent Pain Solutions
What is a Spinal Cord Stimulator?
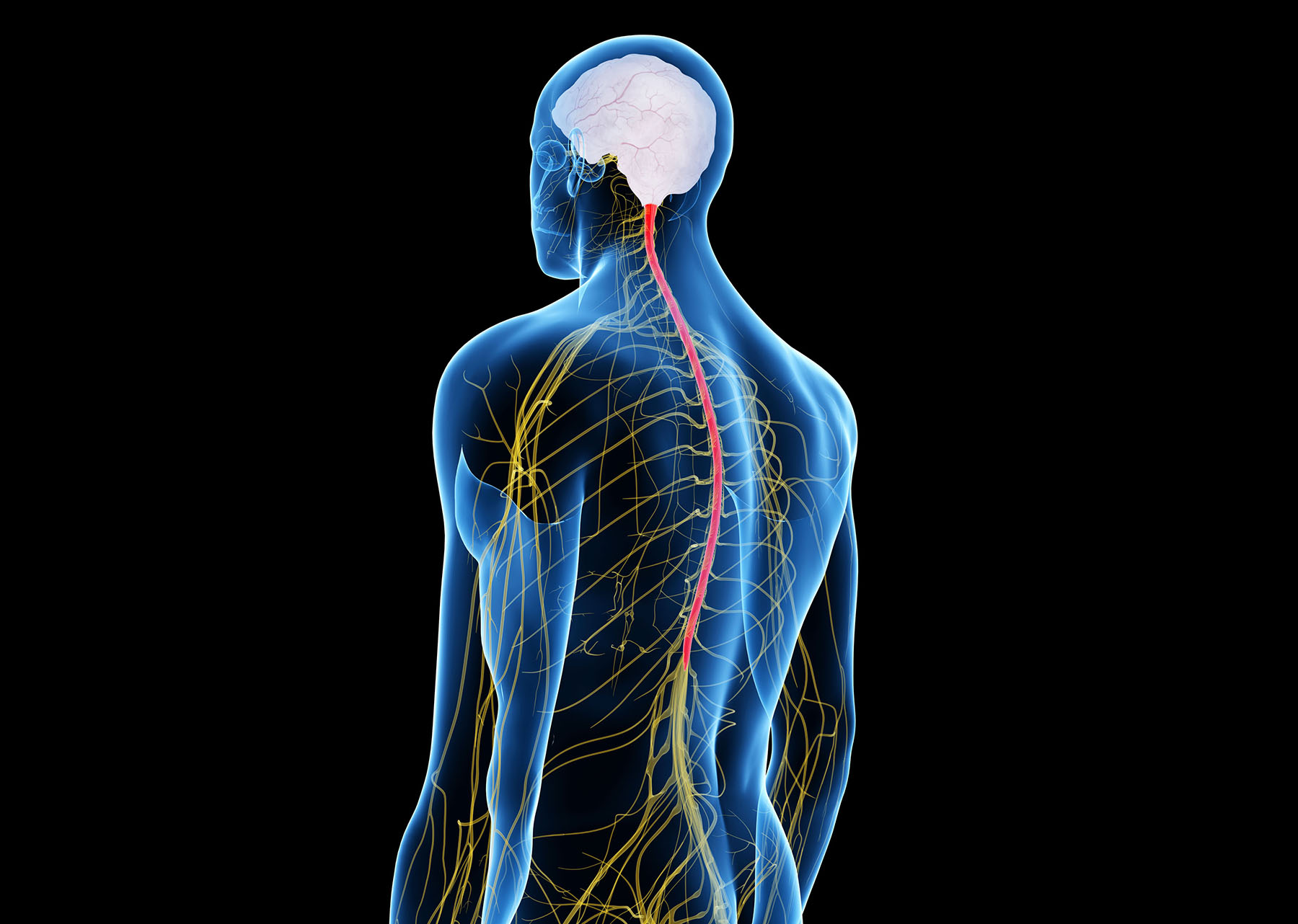
A spinal cord stimulator or SCS is a medical device used to manage chronic pain.
It works by delivering mild electrical impulses to the spinal cord, interfering with the transmission of pain signals to the brain.
The SCS device consists of several components:
- Electrodes. Thin wires, called leads, with electrodes attached to their tips are implanted along the spinal cord or in the epidural space near the spinal cord.
- Generator. A small, battery-powered generator device is typically implanted under the skin of the abdomen or buttocks. This generator produces the electrical impulses delivered by the electrodes.
- Remote Control. Patients can control the intensity and frequency of the electrical impulses using a handheld remote control device.
The electrical impulses produced by the spinal cord stimulator interfere with the transmission of pain signals, essentially masking or overriding the sensation of pain.
This can provide relief for patients suffering from chronic pain conditions such as persistent post spinal surgery syndrome, complex regional pain syndrome, neuropathic pain, and other conditions where traditional pain management methods have been ineffective.
Before undergoing spinal cord stimulator implantation, patients undergo a trial period during which temporary electrodes are placed to assess the effectiveness of the stimulation in reducing pain.
If the trial is successful and provides significant pain relief, the permanent implantation of the electrodes and generator is considered.
Getting an SCS is recommended only for patients who have not responded well to other conservative treatments for chronic pain.
Like any medical intervention, spinal cord stimulation carries potential risks and complications, which should be discussed thoroughly with your doctor before any treatment.
How Does Spinal Cord Stimulation Alleviate Chronic Pain?
Spinal cord stimulation or SCS devices alleviate chronic pain by modulating the transmission of pain signals along the spinal cord.
Here’s how it works:
- Electrical Stimulation. SCS involves the use of a device that delivers mild electrical pulses to specific nerves along the spinal cord. These electrical pulses are generated by an implanted pulse generator and are transmitted through thin wires called leads or electrodes, which are placed in the epidural space near the spinal cord.
- Gate Control Theory. One theory behind the mechanism of SCS is the gate control theory of pain. According to this theory, the electrical stimulation from the SCS device activates large nerve fibres that carry non-painful sensations. These large nerve fibres can “close the gate” to the transmission of pain signals carried by smaller nerve fibres, effectively reducing the perception of pain.
- Pain Signal Interference. Another proposed mechanism is that the electrical pulses from the SCS device interfere with the transmission of pain signals along the spinal cord. By disrupting the normal patterns of pain signal transmission, SCS can reduce the perception of pain in the brain.
- Release of Neurotransmitters. Electrical stimulation from SCS may also trigger the release of neurotransmitters, such as endorphins and serotonin, which are natural pain-relieving chemicals produced by the body. These neurotransmitters can help dampen the perception of pain and promote feelings of well-being.
- Neuromodulation. SCS falls under the broader category of neuromodulation, which involves the alteration of nerve activity through the application of electrical or chemical stimulation. By modulating nerve activity, SCS can effectively manage chronic pain associated with various conditions, including persistent post surgery syndrome, complex regional pain syndrome, neuropathic pain, and other chronic pain disorders.
Overall, spinal cord stimulation offers a non-destructive, reversible method for managing chronic pain that has not responded well to other conservative treatments.
It provides a pain relief option that can improve your quality of life and reduce reliance on medications or invasive procedures.
Why Would You Get a Spinal Cord Stimulator for Chronic Pain?
Spinal cord stimulators (SCS) are often considered for chronic pain management when other treatments have been ineffective or have caused significant side effects.
Here are some reasons why someone might choose to undergo SCS for chronic pain:
- Failed Conservative Treatments. If you have tried and failed to find relief from chronic pain through conservative treatments such as medications, physical therapy, and injections, SCS may be a good alternative.
- Avoiding Surgery. SCS offers a less invasive option compared to surgical interventions such as spinal fusion or laminectomy. Patients who want to avoid the risks and lengthy recovery associated with surgery may prefer to get a spinal cord stimulator implanted.
- Reversible Therapy. Spinal cord stimulation is a reversible procedure with removal of device possible if required in the future.
- Improved Pain Management. SCS can provide significant relief for chronic pain conditions that have not responded well to other treatments. It may help reduce pain intensity, improve function, and enhance overall quality of life.
- Reduced Dependency on Medications. Some individuals may seek SCS to reduce their reliance on pain medications, particularly opioids, which can have significant side effects and risks of addiction.
- Targeted Pain Relief. SCS allows for targeted pain relief, as the electrical stimulation can be adjusted to target specific areas of pain along the spinal cord. This customisation can provide more effective pain management compared to systemic medications.
- Preservation of Function. Chronic pain can significantly impact daily activities and quality of life. By effectively managing pain with SCS, you may be better able to maintain your independence and participate in activities you most enjoy.
- Psychological Well-Being. Chronic pain can have a profound impact on mental health, leading to anxiety, depression, and decreased quality of life. SCS can help improve your psychological well-being by reducing pain and enhancing coping mechanisms.
- Long-Term Pain Management. Unlike some other interventions that may provide temporary relief, SCS offers long-term pain management for chronic conditions. With proper maintenance and adjustments, SCS can continue to provide relief for many years.
Overall, the decision to get a spinal cord stimulator implant for chronic pain is based on your unique circumstances, preferences, and the recommendation of healthcare professionals.
The Risks of Getting a Spinal Cord Stimulator
The decision to undergo spinal cord stimulator (SCS) implantation is significant, as with any medical procedure, it carries potential risks.
While these devices can be highly effective in managing chronic pain for many individuals, it’s essential to be aware of the possible complications and adverse effects.
Here are some common risks associated with getting a spinal cord stimulator:
- Infection. Any surgical procedure carries a risk of infection. Despite precautions taken during the surgery, there is still a possibility of developing an infection at the site of implantation. The infection can also travel into the spinal cord with very rarely, risk of epidural abscess and meningitis.
- Bleeding. Blood loss is a potential risk during the implantation procedure, which may necessitate additional intervention to control bleeding. This includes an epidural haematoma.
- Pain at the Implantation Site. It’s common to experience discomfort or pain at the location where the electrodes and generator are implanted. This pain is usually temporary but can persist for some patients.
- Pocket site complications. Some patients may suffer from complications at the site of the battery such as pain, infection, bleeding, seroma and sensation of heat. This may require removal of the entire device (if infection) or change of the battery site to reduce the symptoms of pain and discomfort.
- Lead Migration. The electrodes placed along the spinal cord may shift or migrate over time, disconnect from the battery or fracture leading to a decrease in pain relief or discomfort. Additional surgery may be required to reposition the leads.
- Device Malfunction. Spinal cord stimulator devices are sophisticated electronic devices, and like any electronic device, they can malfunction. This could result in changes in stimulation patterns or failure to provide pain relief.
- Habituation. Although rare, some patients may have diminished effect from the device over a period of time requiring reprogramming. Sometimes the device may need to be explanted due to lack of benefit.
- Allergic Reaction. Some patients may experience allergic reactions to the materials used in the spinal cord stimulator components, leading to inflammation or discomfort.
- Nerve Damage. During the implantation procedure, there is a risk of damaging nearby nerves, which could result in new or worsening symptoms, numbness or weakness.
- Spinal cord damage. This is a very rare complication of the device resulting in temporary or permanent damage causing weakness, paralysis, numbness, bowel abd bladder dysfunction.
- Dural Puncture. There is a small risk of unintentional puncture of the dura mater (the membrane surrounding the spinal cord), leading to cerebrospinal fluid leakage and subsequent headaches.
- Side Effects. Certain side effects may occur due to the stimulation itself, such as tingling sensations, muscle twitching, or discomfort due to overstimulation.
- Scar Tissue Formation. Scar tissue can develop around the implanted electrodes or generator, potentially impacting the effectiveness of the stimulation or causing discomfort.
- Psychological Effects. Adjusting to life with a spinal cord stimulator can have psychological implications, including feelings of dependency on the device or frustration if pain relief expectations are not met.
- Failure. There are some rare situations when a patient will experience positive benefit from the trial but is unable to achieve a significant benefit from the permanent implant. In these instances, an attempt at programming is made for 6 months and if there is no success, the implant is removed.
If you’re considering having a spinal cord stimulator implanted, it is essential to discuss these potential risks with your doctor.
While a spinal cord stimulator can offer significant pain relief, understanding the risks involved is essential for making an informed decision about your treatment options.
Additional Issues to Consider With a Spinal Cord Stimulator Implant
- MRI compatibility. SCS are generally MRI conditional. This means that most patients can obtain MRIs after the device is placed at a specific radiology clinic which has experience with such devices. You can contact your medical device representative or Dr Mittal for recommendation of a suitable radiology clinic that can perform the MRI. Rarely, the device needs to be removed to obtain specific forms of MRI images depending on the underlying pathology. (for eg, MRIs for brain aneurysms).
- Recharging of the device. There are two types of batteries that may be used: Rechargeable or Non-rechargeable. The rechargeable batteries will require regular recharging either daily, every few days or weekly depending on the energy consumption.
- Battery change. The IPG battery will require changing every 5-10 years depending on the energy consumption. This is usually a day case procedure performed under sedation anaesthesia.
- Driving. During the trial phase, you are not allowed to drive. After the permanent implantation, driving may be commenced only 6 weeks after the surgery. There are stimulation programs that may need to be turned off whilst driving (for eg: tonic stimulation). This is accommodated with other programs that can be used whilst driving instead.
- Travel. Dr Mittal does not recommend travel for the first 3-4 months after the procedure to allow for monitoring and programming of the device. When resuming travel, you will be provided with a ‘device card’ since the device will often ‘beep’ when moving through a metal detector at the airport.
- Exercise. During the trial period, you are restricted from certain movements such as raising arms above shoulder height, heavy lifting and forward bending. This is to avoid migration of the electrode leads. After the permanent implant, you are strongly recommended to follow the same restrictions for 3 months after the implant to allow for enough scar formation to prevent lead migration. During the first 3 months, you are allowed to walk on a regular basis for exercise. After three months, you may commence physiotherapy, hydrotherapy and weight training.
- Swimming. You are recommended not to engage in swimming or utilise a public pool or spa during the trial period. This is to minimise the risk of infection. After the permanent implant, these restrictions continue for the first 3 months after the procedure. Following this, you may recommence swimming and hydrotherapy.
- Activity. Once the device is working well and you are beyond the three month period, you may engage in any form of activity (such as running, jogging, walking, bike riding, weight training, swimming). However some activities are best avoided to prevent lead migration or fracture – these include high impact sports like playing footy, bungee jumping or scuba diving.
The Process of Getting a Spinal Cord Stimulator Implanted
Getting a spinal cord stimulator placed consists of two stages.
- The Trial Phase
- The Permanent Implantation Phase
The above involve two separate procedures performed on two different days or in separate appointments in hospital under anaesthesia.
In the initial stage, electrodes are implanted along the targeted area of the spinal cord, with the wire ends extending above the skin, ready to connect to the device.
During this phase, a small incision is made in the back, and electrodes are carefully inserted using a needle. Patients are typically hospitalised overnight after this step.
The electrodes are then linked to a portable stimulation device for ten to fourteen days, during which the effectiveness of the stimulator is evaluated.
These electrodes are completely removed on Day 14 under sterile technique, in clinic by the pain physician.
If significant pain reduction is observed, the second stage involves the permanent placement beneath the skin of a miniature stimulator, known as an implantable pulse generator or IPG. It’s equipped with a battery.
Usually located in the lower back or buttocks, this is a permanent fixture, with rechargeable batteries designed for extended lifespan, ranging from five to ten years based on stimulator settings
- Initial Trial Electrodes:
- This procedure is performed under sedation anaesthesia in a hospital setting.
- Your skin is sterilised at the injection site, and a local anaesthetic is administered to numb the area.
- Wires (leads) are inserted through a needle and placed in the epidural space in the target region by your pain management physician. X Ray guidance is used to accurately place the leads depending on the location. There are NO incisions made on the skin during this phase.
- These leads are connected externally to a smartphone-sized electrical pulse generator, which you carry with you during the initial test period to assess the treatment’s effectiveness.
- You are generally required to stay overnight in hospital for monitoring with discharge and programming of the device commencing the next morning.
- The device is programmed and trialled for a 7-14 days period as an outpatient. You are then reviewed in the clinic where your doctor will remove the electrodes under sterile technique. This then concludes the trial.
- Permanent Neurostimulator Implant
- This surgery is performed under general anaesthesia, with you lying on your stomach. You are required to stay in hospital for 1-2 days post procedure.
- Your skin is sterilised at the surgical site.
- General anaesthesia is administered to ensure you are unconscious and pain-free during the procedure.
- Your pain management physician implants the electrodes in the epidural space and the IPG battery under your skin for long-term pain management. You can expect three 3-5 cm skin incisions as a result of the procedure.
This pair of procedures allows for a comprehensive evaluation of the effectiveness of spinal cord stimulation before committing to a permanent implant.
The initial trial period with external leads helps determine if the treatment provides sufficient pain relief, while the second procedure involves the implantation of a permanent device for ongoing management if the initial trial is successful.
Preparing for a Spinal Cord Stimulator
At the Persistent Pain Solutions Clinic, we recommend that you complete both a pain chart and a pain diary over the course of a week or so prior to your procedure.
The pain chart will help identify the areas of your body affected areas, while the pain diary tracks your daily pain levels, including any fluctuations.
To ensure the safety and efficacy of the procedure, we advise against undergoing any other medical interventions, such as dental treatments or colonoscopies, 48 hours before or after the procedure.
You will also be provided with a full body antiseptic preparation to be applied in the few days prior to the procedure to minimise the risk of infection.
To further reduce the risk of infection, you will be advised to stop smoking 6 weeks prior to the procedure and maintain strict control of your blood sugar levels if you have diabetes.
Depending on your BMI, you may be advised to lose some weight before proceeding with the trial once again to minimise the risk of infection but also the risk of anaesthesia.
Occasionally, patients will require a review by an infectious disease physician to obtain further advice to manage perioperative risk of infection.
Please refrain from eating or drinking for six hours prior to the procedure, except for taking necessary medication with small sips of water.
Please inform the pain physician if you are taking diabetes medications, weight loss or blood thinning medications.
You will be advised how to manage these medications in the perioperative period by your treating doctor.
Before the procedure, please inform your team if you have any allergies, high blood pressure, a history of bleeding or blood clotting issues, have a pacemaker or defibrillator, are taking antibiotics, or are otherwise feeling unwell.
Please arrange for transportation to and from the appointment — driving yourself afterwards is not recommended.
After Getting a Spinal Cord Stimulator Permanent Implant (Follow-Up)
Following the spinal cord stimulator procedure, you can expect to remain hospitalised for one or two days.
Complete recovery may take up to six weeks, during which incorporating gentle daily exercise like walking is recommended.
We’ll provide detailed instructions on the implantable pulse generator and specific activities to avoid.
Post-procedure, anticipate some discomfort at the insertion site for approximately one week.
During this period, refrain from lifting heavy objects and avoid excessive stretching, twisting, or bending beyond 45 degrees. Keep the incision dressing dry and undergo frequent checks for signs of infection.
You may commence driving 6 weeks after the procedure.
Dr Mittal will schedule a follow-up appointment for 10 days after your procedure for incision site review and stitch removal.
You can expect regular follow up reviews with Dr Mittal at 4 weeks and 6-8 weeks after the procedure.
During this time, the wound will be inspected for signs of infection or any other complication and programming of the device shall commence.
Dr Mittal will regularly review you over the first 6 months to ensure the SCS is programmed effectively to provide pain relief, similar to the trial.
After that regular reviews are scheduled every 6 – 12 months depending on the need.
The IPG battery is changed every 5-10 years and usually requires a day case procedure under sedation in a hospital.
Getting a Spinal Cord Stimulator Removed
If you do not experience a significant reduction in pain after getting a spinal cord stimulator, it can be removed in a short procedure.
That said, If your spinal cord stimulator does not provide the expected relief or fails to work adequately, several steps can be taken to address the situation:
- Reevaluation. The first step is to reassess the placement and settings of the spinal cord stimulator. This may involve adjusting the stimulation parameters, reprogramming the device, or repositioning the electrodes to optimise effectiveness.
- Trial of Different Settings. Different stimulation settings and programming adjustments can be tried to determine if alternative configurations provide better pain relief.
- Revision Surgery. In some cases, revision surgery may be necessary to reposition the electrodes, replace malfunctioning components, or address any issues contributing to the lack of efficacy.
- Exploration of Alternative Therapies. If spinal cord stimulation is not providing satisfactory pain relief, alternative pain management strategies may be explored. This could include trying different medications, physical therapy, cognitive-behavioural therapy, or other interventional procedures.
- Exploring Other Neuromodulation Techniques. If spinal cord stimulation is not effective, other neuromodulation techniques such as peripheral nerve stimulation or dorsal root ganglion stimulation may be considered.
- Managing Expectations. It’s important for you and your doctor to communicate openly about expectations and goals for pain management. Sometimes, realistic expectations may need to be adjusted based on individual circumstances and response to treatment.
Finding a Doctor Who Performs Spinal Cord Stimulation Near You
Finding a doctor who provides spinal cord stimulation in Melbourne or elsewhere in Australia is a key first step towards reducing or managing your refractory chronic pain condition.
Work with your general practitioner to get a referral to a pain management physician who offers spinal cord stimulators or similar procedures for chronic neuropathic pain.
You can also research pain management clinics online or speak to family members, friends, or support groups (both online and in real life) for recommendations from those who have dealt with similar chronic pain challenges.
Spinal Cord Stimulation at Persistent Pain Solutions
Persistent Pain Solutions is a pain management clinic in Melbourne, Australia that provides spinal cord stimulators to chronic pain patients who wish to avoid surgical interventions or more invasive treatments.
If you have a chronic pain condition that is not responding to other treatments, reach out to the team at Persistent Pain Solutions.
Dr Mittal and her team will work with you to determine if getting a spinal cord stimulator is right for your needs and otherwise help create a pain management plan that improves your quality of life.

Find a Persistent Pain Solutions Location Near You
Leader in Personalised Care, Integrative Pain Medicine, & Pain Management Intervention.
Pain Treatments We Offer in Melbourne, Victoria

Don’t Miss an Update
Join our newsletter to learn more about our staff, patients, and communities in the know on all of the recent news, events, and announcements for Persistent Pain Solutions.